As the most common equipment in clinical practice, multi-parameter patient monitor is a kind of biological signal for long-term, multi-parameter detection of physiological and pathological status of patients in critical patients, and through real-time and automatic analysis and processing, timely transformation into visual information, automatic alarm and automatic recording of potentially life-threatening events. In addition to measuring and monitoring the physiological parameters of patients, it can also monitor and deal with the status of patients before and after medication and surgery, timely discover the changes in the condition of critically ill patients, and provide a basic basis for doctors to correctly diagnose and formulate medical plans, thus greatly reducing the mortality of critically ill patients.


With the development of technology, the monitoring items of multi-parameter patient monitors have expanded from the circulatory system to respiratory, nervous, metabolic and other systems. The module is also expanded from the commonly used ECG module (ECG), respiratory module (RESP), blood oxygen saturation module (SpO2), noninvasive blood pressure module (NIBP) to temperature module (TEMP), invasive blood pressure module (IBP), cardiac displacement module (C.O), noninvasive continuous cardiac displacement module (ICG), and end-breath carbon dioxide module (EtCO2) ), electroencephalogram monitoring module (EEG), anesthesia gas monitoring module (AG), transcutaneous gas monitoring module, anesthesia depth monitoring module (BIS), muscle relaxation monitoring module (NMT), hemodynamics monitoring module (PiCCO), respiratory mechanics module.


Next, it will be divided into several parts to introduce the physiological basis, principle, development and application of each module. Let's start with the electrocardiogram module (ECG).
1: The mechanism of electrocardiogram production
Cardiomyocytes distributed in the sinus node, atrioventricular junction, atrioventricular tract and its branches generate electrical activity during excitation and generate electric fields in the body. Placing a metal probe electrode in this electric field (anywhere in the body) can record a weak current. The electric field changes continuously as the period of motion changes.
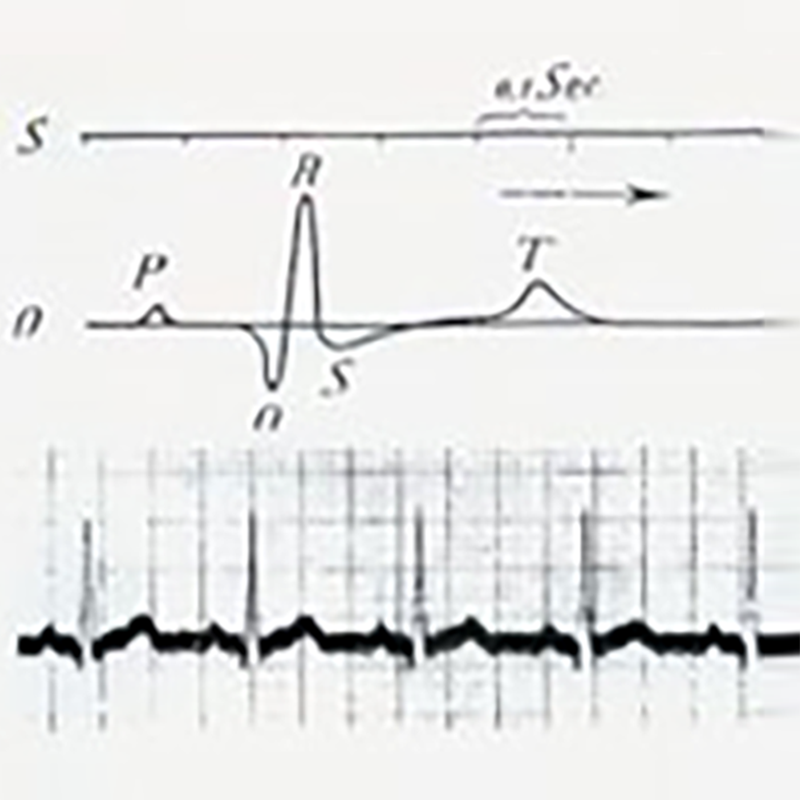
Because of the different electrical properties of tissues and different parts of the body, the exploration electrodes in different parts recorded different potential changes in each cardiac cycle. These small potential changes are amplified and recorded by an electrocardiograph, and the resulting pattern is called an electrocardio-gram (ECG). The traditional electrocardiogram is recorded from the surface of the body, called the surface electrocardiogram.
2:History of electrocardiogram technology
In 1887, Waller, professor of physiology at Mary's Hospital of the Royal Society of England, successfully recorded the first case of human electrocardiogram with a capillary electrometer, although only V1 and V2 waves of the ventricle were recorded in the figure, and atrial P waves were not recorded. But Waller's great and fruitful work inspired Willem Einthoven, who was in the audience, and laid the groundwork for the eventual introduction of electrocardiogram technology.
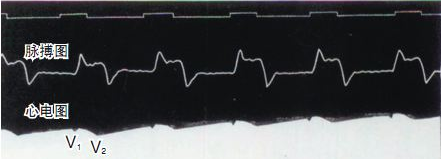
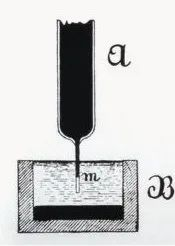
------------------------(AugustusDisire Walle)---------------------------------------(Waller recorded the first human electrocardiogram)-------------------------------------------------(Capillary electrometer )-----------
For the next 13 years, Einthoven devoted himself entirely to the study of electrocardiograms recorded by capillary electrometers. He improved a number of key techniques, successfully using string galvanometer, body surface electrocardiogram recorded on the photosensitive film, he recorded the electrocardiogram showed the atrial P wave, ventricular depolarization B, C and repolarization D wave. In 1903, electrocardiograms began to be used clinically. In 1906, Einthoven recorded the electrocardiograms of atrial fibrillation, atrial flutter and ventricular premature beat successively. In 1924, Einthoven was awarded the Nobel Prize in Medicine for his invention of electrocardiogram recording.
---------------------------------------------------------------------------------------True complete electrocardiogram recorded by Einthoven----------------------------------------------------------------------------------------------------------
3:Development and principle of lead system
In 1906, Einthoven proposed the concept of bipolar limb lead. After connecting recording electrodes in the right arm, left arm and left leg of patients in pairs, he could record bipolar limb lead electrocardiogram (lead I, lead II and lead III) with high amplitude and stable pattern. In 1913, the bipolar standard limb conduction electrocardiogram was officially introduced, and it was used alone for 20 years.
In 1933, Wilson finally completed the unipolar lead electrocardiogram, which determined the position of zero potential and central electric terminal according to Kirchhoff's current law, and established the 12-lead system of Wilson network.
However, in Wilson's 12-lead system, the electrocardiogram waveform amplitude of the 3 unipolar limb leads VL, VR and VF is low, which is not easy to measure and observe changes. In 1942, Goldberger conducted further research, resulting in the unipolar pressurized limb leads that are still in use today: aVL, aVR, and aVF leads.
At this point, the standard 12-lead system for recording ECG was introduced: 3 bipolar limb leads (Ⅰ, Ⅱ, Ⅲ, Einthoven, 1913), 6 unipolar breast leads (V1-V6, Wilson, 1933), and 3 unipolar compression limb leads (aVL, aVR, aVF, Goldberger, 1942).
4:How to get good ECG signal
1. Skin preparation. Since the skin is a poor conductor, proper treatment of the patient's skin where the electrodes are placed is necessary to obtain good ECG electrical signals. Choose flat ones with less muscle
The skin should be treated according to the following methods: ① Remove the body hair where the electrode is placed. Gently rub the skin where the electrode is placed to remove dead skin cells. ③ Wash the skin thoroughly with soapy water (do not use ether and pure alcohol, because this will increase the resistance of the skin). ④ Allow the skin to dry completely before placing the electrode. ⑤ Install clamps or buttons before placing the electrodes on the patient.
2. Pay attention to the maintenance of the cardiac conductance wire, prohibit winding and knotting the lead wire, prevent the shielding layer of the lead wire from being damaged, and timely clean up the dirt on the lead clip or buckle to prevent lead oxidation.
Post time: Oct-12-2023



